Every 15 minute increase in door to needle times after 60 minutes of hospital arrival was significantly associated with higher cardiovascular readmission secondary outcome adjusted hr 1 02 95 ci 1 01 1 04 and higher stroke readmission a post hoc secondary out come adjusted hr 1 02 95 ci 1 00 1 04.
Door to needle time in acute stroke.
Question is there an association between shorter door to needle time with thrombolytic therapy and long term mortality and hospital readmission in patients with acute ischemic stroke.
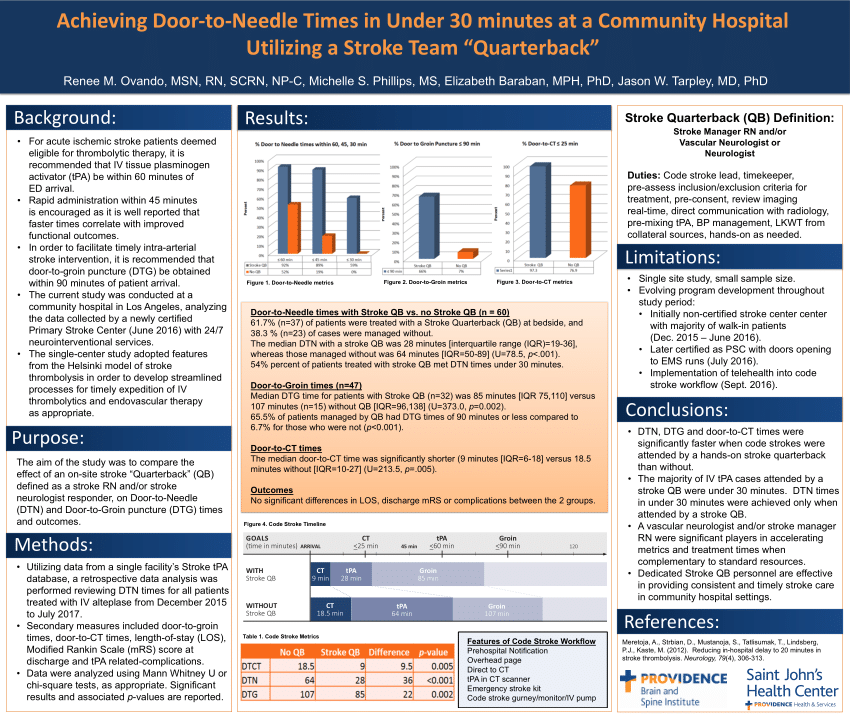
The benefits of intravenous tissue type plasminogen activator tpa in acute ischemic stroke are time dependent and guidelines recommend a door to needle time of 60 minutes.
However fewer than one third of acute ischemic stroke patients who receive tpa are treated within guideline recommended door to needle times.
The benefits of tpa in patients with acute ischemic stroke are time dependent and guidelines recommend a door to needle time.
A national institute of neurological disorders and stroke national symposium on the rapid identification and treatment of acute stroke recommended a door to needle target time of 60 minutes.
Lowering the median dnt is an essential goal for quality improvement and is therefore used worldwide in audits for this.
Man s et al association between thrombolytic door to needle time and 1 year mortality and readmission in patients with acute ischemic stroke jama 2020.
8 aha asa guidelines recommend the target for completion of initial evaluation and start of tpa treatment should be within 1 hour of the patient s arrival.
However these associations.